THE SENSITIVITY AND SPECIFICITY OF ULTRASOUND FOR THE DIAGNOSIS OF CARPAL TUNNEL SYNDROME: A META-ANALYSIS
Filed under Diagnoses
Fowler, J. R., Gaughan J. P., & Ilyas, A.M. (2011). The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: A meta-analysis. Clinical Orthopedics and Related Research, 469(4), 1089-1094.
The Skinny –The authors sought out to determine the sensitivity and specificity of ultrasound therapy for the diagnosis of carpal tunnel syndrome using three scenarios. 1.) using all studies regardless of reference standard 2.) using all studies with electrodiagnostic as the reference standards and 3.) using all studies with clinical diagnosis as the gold standard.
In the Weeds – The authors found a total of 19 articles that were included in the review. Remember, sensitivity indicates a true positive rate and specificity indicates a true-negative rate.
They found the sensitivity and specificity of ultrasound was 77.6% (71.6%-83.6%) and 86.8% (78.9%-94.8%), respectively.
They found the sensitivity and specificity of electrodiagnostic testing to be 80.2% (71.3-89.0) and 78.7% (66.4-91.1, respectively).
Bringing it Home– Ultrasound showed a higher specificity but electrodiagnostic had a slightly higher sensitivity. Although ultrasound may not replace electrodiagnostic testing as the most sensitive tool for diagnosing carpal tunnel, it may be a feasible alternative to electrodiagnostic testing as a first line confirmatory test.
Overall a very nicely done study however it was not without its limitation. There was a lack of heterogeneity among the studies reviewed. Both, ultrasound and electrodiagnostic testing it very operator dependent. The upside of ultrasound is it can be performed very quickly, it is often less expensive, and off course it is essentially pain-free.
–
More To Read
What is the Effectiveness of IASTM?
Citation Kim, J., Sung, D. J., Lee, J. (2017). Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: Mechanisms and practical application. Journal of Exercise Rehabilitation, 13(1). doi: https://doi.org/10.12965/jer.1732824.412 The skinny IASTM is a relatively simple technique that uses the surface of an instrument to minimize the amount of pressure or force needed…
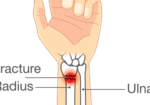
Is therapy needed after a distal radius fracture?
Coughlin T, Norrish AR, Scammell BE, Matthews PA, Nightingale J, Ollivere BJ. Comparison of rehabilitation interventions in nonoperatively treated distal radius fractures: a randomized controlled trial of effectiveness. Bone Joint J. 2021Jun;103-B(6):1033-1039. doi: 10.1302/0301-620X.103B.BJJ-2020-2026.R1.Epub 2021 Apr 30. PMID: 33926211. The Skinny: Individuals with distal radius fractures are very common in the hand therapy world. This…
Functional Home Exercises for Patients with Wrist Instability
Functional Home Exercises for Patients with Wrist Instability Ever wondered what brushing your teeth, dressing, making a U-turn, and playing sports have in common? They all rely on a stable wrist. Wrist stability is crucial for everyday activities, supporting wrist proprioception, coordination, motor control, stability, and mobility (Wietlisbach, 2019). For patients recovering from a wrist…
Carpal Fractures: A Brief Overview
Carpal fractures account for 8% of fractures in the upper extremity. The carpals are situated between the (distal radius and ulna) and the metacarpals. They make up the proximal row- Scaphoid, Lunate, Triquetrum, and Pisiform, the distal row- Trapezium, Trapezoid, Capitate, and Hamate. Here are some of the most common carpal bone fracture Scaphoid…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.