It was early in my career, maybe a year out of school. I was working with a veteran physical therapist that had been practicing for thirty plus years. She was somewhat intimidating and one of those old school physical therapists that thrived on being aggressive. We were chatting about what areas of occupational hand therapy I was interested in. I told her I was interested in hand therapy.
She said to me, “why would you ever want to be a table-top therapist?”
That very question has followed me in my career and in some ways has driven me to make sure I am providing treatments that are centered around “occupation” and to ensure I am providing meaningful therapy.

I also have this amazing opportunity to work with several students from the local university where occupation is the center of their education. It is the foundation for occupational therapy and what makes us different from the other rehabilitative profession.
It is not only about treating occupation and a means to an end but also as the end. How can you possibly provide occupation-based treatment when you are concerned about the details of a tendon gliding 3-5 mm without rupturing but preventing scar adhesions. How can you make passive flexion exercises occupation based? How is this an occupation-based treatment? I think it is about keeping occupation at the core of the treatment.
As a simple illustration, I have provided a simple case study that is typical for our clinic.
A 26-year-old patient was helping some friends do some remodeling when her wrists went through a glass window. She lacerated every flexor tendon along with both her median and ulnar nerve. She is a young mother of three and unemployed. Her fiancé just got done serving 5 years of a prison sentence for armed robbery. Her two older children are in the custody of another family member and her youngest is living with her and the fiancé.
During the initial evaluation, my questions are centered around occupation. What does a typical day look like before the injury? What does it look like now that you have no use of your dominant hand? What are your current goals? What things do you need to be able to do now to get through the day?

Getting an understanding of the daily occupations, gives me insight into the patient’s life and how my treatments can not only prevent tendon ruptures but provide a meaningful treatment the patient can implement immediately. On the first visit, we did review edema management techniques along with a protected range of motion exercises. I was able to help her identify times she could implement these exercises based on what she told me during the initial evaluation. I was able to show her one-handed techniques (one handed techniques occupational therapy) to complete the ADLs that were crucial to making her day easier such as donning a bra, doing her daughters hair and doing simple meal preparation for her family.
Occupation in hand therapy can not only be used as a means to an end but also as a therapeutic agent throughout the intervention.
What are some other ways you can implement occupation-based treatment into hand therapy?
More To Read
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy As hand therapists we often encounter patients presenting with swollen arms, hands, and/ or fingers, often attributing these symptoms to various conditions. Two commonly confused terms in this area are “edema” and “lymphedema.” While both involve swelling, they have distinct causes, presentations,…
Pain management techniques for Wrist Fractures
Pain management techniques for wrist fractures Distal radius fractures account for 17.5% of all fractures with a median age of 60.23(Candela et.al, 2022). Pain management is a significant part of post wrist fracturetreatment due to limitations that pain incurs. Chronic Regional Pain Syndrome (CRPS) canoccur along with a distal radius fracture but will not be…
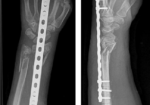
Outcomes of Dorsal Bridging Plates
Outcomes of Dorsal Bridging Plates Fares, A. B., Childs, B. R., Polmear, M. M., Clark, D. M., Nesti, L. J., & Dunn, J. C. (2021). Dorsal Bridge Plate for Distal Radius Fractures: A Systematic Review. The Journal of Hand Surgery. https://doi-org.methodistlibrary.idm.oclc.org/10.1016/j.jhsa.2020.11.026 The Skinny Distal radius fractures (DRF) are a common injury that we see in…
Mirror therapy after a peripheral nerve repair in hand therapy
Rapid Review Paula, M. H., Barbosa, R. I., Marcolino, A. M., Elui, V. M., Rosén, B., & Fonseca, M. C. (2016). Early sensory re-education of the hand after a peripheral nerve repair based on mirror therapy: a randomized controlled trial. Brazilian journal of physical therapy, 20(1), 58–65. https://doi.org/10.1590/bjpt-rbf.2014.0130 The Skinny: Therapy is often provided following an…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.