Teo, S. H., Ng D. C., Wong, Y.K.(2018). Effectiveness of proximal interphalangeal joint blocking orthosis vs metacarpophalangeal joint blocking orthosis in trigger digit: A randomized clinical trial. Journal of Hand Therapy, 1-7.
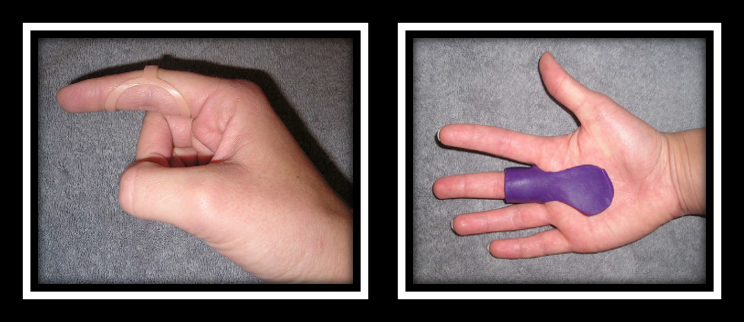
The Skinny- This study compared PIP joint immobilization via an Oval-8TM with a custom MCP blocking orthosis in the treatment of trigger finger.
In the Weeds – Patient (n=35) with Trigger Finger (n=43) were analyzed. Twenty-three patients were allocated to the PIP joint splinting group and 20 patients were in the MCP splinting group. Patients wore the orthosis for eight weeks.
Pain reduction was observed in both groups, but pain reduction was greater with PIP joint splinting compared to the MCP joint splinting group (MCP joint splint). There was only significant improvement in QuickDASH for the PIP splinting Group. Patients wore the pip joint splint significantly longer during the day compared to the MCP splinting group (MCP splint), most likely due to improved comfort.
Bringing it Home- Findings suggest both orthoses are effective in reducing QuickDASH scores, reducing pain and improving overall trigger finger symptoms based on Green’s Classification. However, the pip joint immobilization splint was better for improved function and improved compliance.
The rationale for the rating. Small sample size. All patients with comorbidities were excluded limiting the generalizability of findings. Immobilizing the PIP joint compared to the MCP allows more function and improved compliance. When immobilizing the MCP you limit intrinsic grasp which is a necessity for function. The authors recommend wearing the orthosis for a 4-week duration of 24 hours in order to reduce triggering symptoms followed by night-time splint wear for another 3-4 weeks.
4 Comments
Leave a Comment
More To Read
5 return-to-cooking activities (that don’t require a kitchen)
Hand therapy can and should be very occupation-based. Every week, we hear comments from patients that back that statement up: “I need to get back to work” “I just want to golf again” “I can’t even open a water bottle” “My spouse has to do all of the cooking” Although standard exercises are helpful, it’s…
Trigger Finger… Quick and Dirty!
This is for you… Hand Therapists! Stenosing tenosynovitis, otherwise known as trigger finger, is a common condition affecting children and adults of all ages. Fast Facts Trigger finger usually occurs at the A1 pulley It occurs with inflammation of the tendons and sheaths of fds and fdp The digit can lock in both flexion and…
The 4 Stages of Simple Wound Care in Hand Therapy
Wound care is messy. It can be intimidating and scary. With so many variations of wounds (for example, white skin around wound) and so many products out there it is hard to know what to use, when to use it, and how to use it. If you go to a wound care conference, you’ll spend most…
Video Augmented Hand Therapy after CVA with hemiplegia.
The previous rapid review discussed the positive outcomes of video-augmented hand therapy after a CVA with hemiplegia. Please watch this vlog to discover how to make the video augmented box to make it easily integrated into your clinic. Video By: Shannon Skowbo
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.







Trigger finger is easy to fix with surgery release. I’ve had it done. Piece of cake.
Have seen a pt lose a finger due to a freak release surgery accident. Have seen the scar tissue left behind following a surgical release replicate a trigger digit. Have seen conservative management effectively treat a trigger digit.
Even simple surgeries carry risks for pts, especially if there are preexisting conditions like diabetes or Raynaud’s. So maybe it is best to explore all aspects of treatment before throwing out a blanket statement, right?
why go to surgery before all conservative measures? Before surgery I would certainly consider CSI, which most times resolve the situation. another thing, is inflammation in the body due yo metabolic issues also need to be considered
What are some suggestions for pediatric trigger finger in the thumb?