Coughlin T, Norrish AR, Scammell BE, Matthews PA, Nightingale J, Ollivere BJ. Comparison of rehabilitation interventions in nonoperatively treated distal radius fractures: a randomized controlled trial of effectiveness. Bone Joint J. 2021Jun;103-B(6):1033-1039. doi: 10.1302/0301-620X.103B.BJJ-2020-2026.R1.Epub 2021 Apr 30. PMID: 33926211.
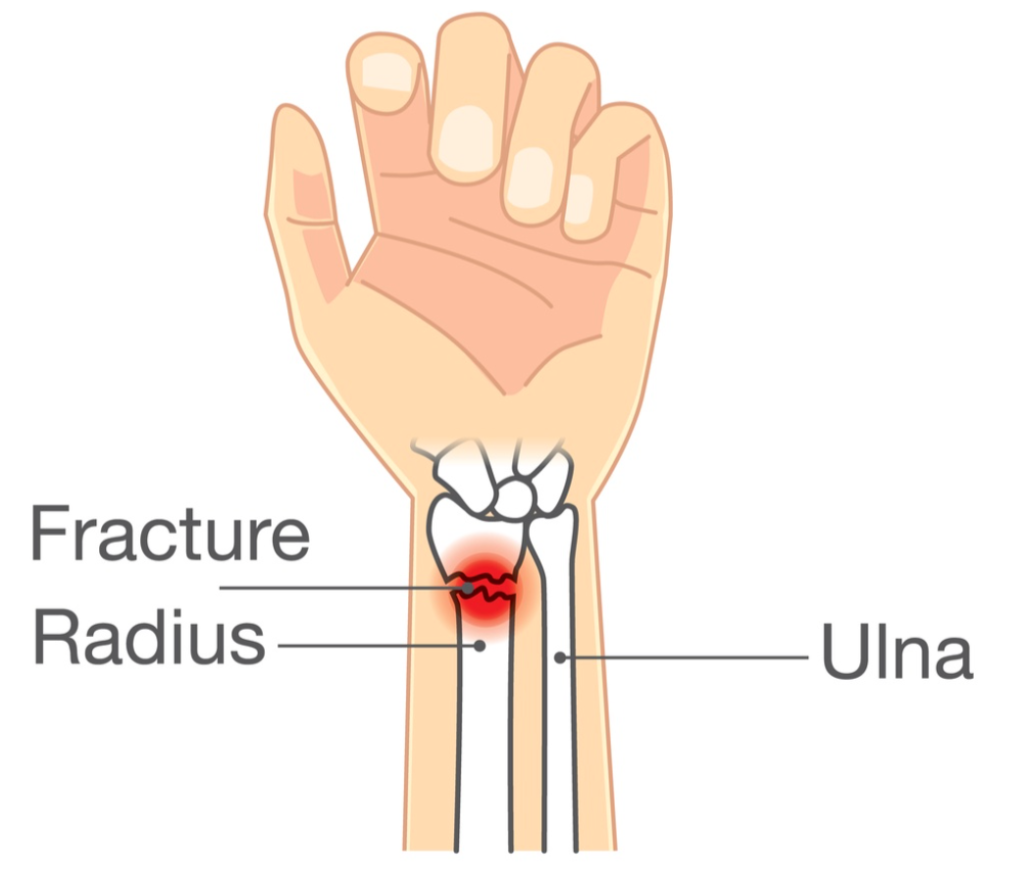
The Skinny: Individuals with distal radius fractures are very common in the hand therapy world. This study sought out to determine whether the presence in therapy is clinically necessary, or if the therapy needs of those with distal radius fractures could be met just as easily with an informational leaflet or video as a part of distal radius fracture rehabilitation.
In the weeds:
This study involved 95 individuals, ages 18 to 70-years, who had been non-operatively treated for distal radius fractures, with casting for 6 weeks. The aim of the study was to compare the effectiveness of hand therapy services that provide distal radius fracture home exercise program vs. an informational leaflet vs. an informational video upon cast removal.
The video and leaflet included instructions on the same seven exercises. The video could be accessed through youtube or with a DVD, over 4 sessions. The traditional face-to-face treatment sessions began after cast removal and lasted for 6–weeks.
The DASH, The DASH-work subscale, wrist ROM, and grip strength measures were taken at baseline, 6-weeks, and 1-year post-intervention. The baseline began after cast removal, which was 5-7 weeks for all participants.
Of the original 120 participants; 21 were lost to follow-up, 30 participants received the advice leaflet, 32 received the advice video, and 33 received face-to-face therapy.
168 patients were excluded from the study due to an array of complications, including post-plaster stiffness, preventing them from placing their hands flat on a tabletop. Of the patients that were included, 15 more were removed from the study due to complications, such as malunions and Dupuytren’s.
Of the outcomes listed above only the DASH-work subscale provided significant differences in favor of face-to-face therapy vs. the leaflet. And those differences were significant at the 6-week mark only.
Bringing it Home:
We have several concerns about this study:
Inclusion/Exclusion: 168 participants were excluded initially with 15 more added to that list as the study progressed. Those with stiffness, malunion, and other exclusion criteria are the very ones who would have benefited most from face-to-face therapy.
Casting Protocol: For the adult population specifically, orthosis use has become the preferred form of protection. Casting places greater limitations on mobility and functional use and may have resulted in increased limitations for all participants in this study. Also, orthoses that are removable also allow for earlier intervention when needed.
Age Range: This group of individuals fell between the ages of 18 and 70, a significant spread. The authors referenced an article by Gutierrez-Espinoza et. al. in which results found that all measures indicate that clients over 60 years of age benefit from in-person visits. It would have been nice to include subcategories statistically analyzed by age to determine the effectiveness by age range and other demographic variables.
Face-to-face Sessions: The authors were unclear on what the face-to-face sessions included. Did this include occupational therapy interventions for distal radius fracture: manual therapy, simple exercises, therapeutic activities, occupational adaptions? Additionally, did the 4 ‘sessions’ with the leaflets or videos include additional interactions? These might also count as in-person interactions if any clarifications were provided. Without specifications included in the article, it is hard to clarify the differences.
Our Rating: 2/5
More research is required in the realm of distal radius fractures, and we respect and appreciate these researchers for adding to the body of knowledge that we do have. However, the conclusion of this study could have heavy implications for many people, and the number of confounding variables and unanswered questions in regards to its methodology limit our rating.
Future research on the effectiveness of distal radius fracture interventions should include: age stratification, detailed information regarding the nature of the face-to-face interventions, and should replace the casting protocol for orthosis fabrication (and earlier intervention).
Gutiérrez-Espinoza H, Rubio-Oyarzún D, Olguín-Huerta C, Gutiérrez-Monclus R, Pinto-Concha S, Gana-Hervias G. Supervised physical therapy vs home exercise program for patients with distal radius fracture: a single-blind randomized clinical study. J Hand Ther. 2017;30(3):242–252.
More To Read
Dorsal Wrist Pain?
Incorporating Emerging Evidence into Clinical Practice for Patients Experiencing Dorsal Wrist Pain During Weight-Bearing Activities By: Brittany Day Supporting Evidence A randomized control study recently published in the Journal of Hand Therapy found rigid carpal stabilizing taping (CST) to significantly increase passive range of motion, active range of motion, and decrease pain in patients experiencing…
Radial Nerve Palsy: A Paralysis Causing Wrist Drop
Radial Nerve Palsy- Treatment
Trigger Finger… Quick and Dirty!
This is for you… Hand Therapists! Stenosing tenosynovitis, otherwise known as trigger finger, is a common condition affecting children and adults of all ages. Fast Facts Trigger finger usually occurs at the A1 pulley It occurs with inflammation of the tendons and sheaths of fds and fdp The digit can lock in both flexion and…
Changes in ROM of the MCP after Trapeziometacarpal Arthrodesis
Rapid Review: Changes in ROM of the MCP after Trapeziometacarpal Arthrodesis Hayashi, M., Kato, H., Komatsu, M., Yamazaki, H., Uchiyama, S., & Takahashi, J. (2021). Changes in the Functional Range of Motion of the Thumb Metacarpophalangeal Joint After Trapeziometacarpal Arthrodesis for Patients With Advanced Trapeziometacarpal Osteoarthritis. The Journal of hand surgery, S0363-5023(21)00613-4. Advance online publication. https://doi.org/10.1016/j.jhsa.2021.09.018. The Skinny: Several published…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






