7 Tips to Help your Patients Manage Hand Osteoarthritis
Filed under Treatments
Our hands are one of the most intricate structures in the human body. They are composed of a network of tendons, ligament and nerves that make it possible to perform daily tasks such as unlocking a door, peeling an egg, or sending an email to a friend. Osteoarthritis in your hands can make these simple tasks very difficult if not impossible.
Osteoarthritis is something that comes and goes, and everyone’s symptoms are different. As a therapist you can help your patients learn what triggers their symptoms, so they can begin to effectively manage their arthritis. These triggers can be anything from the diet they are consuming, the amount of daily stress, their sleep schedule and their daily activities. Here are some basic tips to share with your patients.

1. Maintain Daily Exercise
Have your patients get the recommended daily exercise with a minimum of twenty minutes per day. If walking is not option, often I’ll recommend swimming or cycling which is very low stress on joints.
2. Eat a Healthy, Balanced Diet
Studies have shown that a variety of nutrients may alleviate symptoms. Foods rich in vitamin c such as fruits and vegetable are important to have in your diet. Omega 3 fatty acids found in fish and fish oil may alleviate pain (WebMD, 2018).
3. Understand Inflammation
The greatest damage to joints occurs when patients are in the inflammatory phase. Teaching patients to recognize this phase is crucial to preventing joint destruction and deformity. For example, if you have a patient that is really inflamed in the DIP joint and the joint is painful and red, it is recommending the patient wear a DIP immobilization splint or at a minimum wrap the joint for support. The wrap can be an elastic wrap or a silicone gel sleeve. Also if your patient is having significant thumb pain from OA you can make a custom thumb orthosis.
Sign-up for our CMC Orthosis free training.
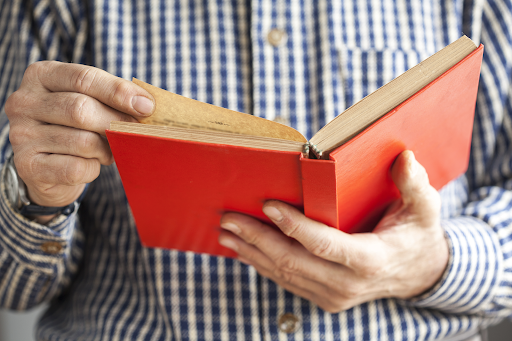
4. Work Smarter, Not Harder
Teaching your patients to use larger joints instead of the small joints. For instance, instead of holding a book with lateral pinch hold book with one hand on bottom and one on top. This can prevent further stress on vulnerable joints.
5. Respect Pain
Pain is your body’s way of protecting itself. When you are having pain, identify the possible reasons for pain and what you can do to change the pain-provoking cause. Also, if you are in pain this typically indicates you are causing joint damage.

6. Use Heat
Teaching patients that heat can improve blood flow, alleviate pain and spasm especially prior to performing range of motion.
7. Keep a diary.
Having patients keep a diary recording their food intake, daily activities, and pain level can be a powerful tool to recognizing triggers.
Teaching self-management techniques for osteoarthritis can be a lifelong gift for your patients. What are some other tips and tricks you can share with your patients? Leave us a comment below!
2 Comments
Leave a Reply Cancel Reply
More To Read
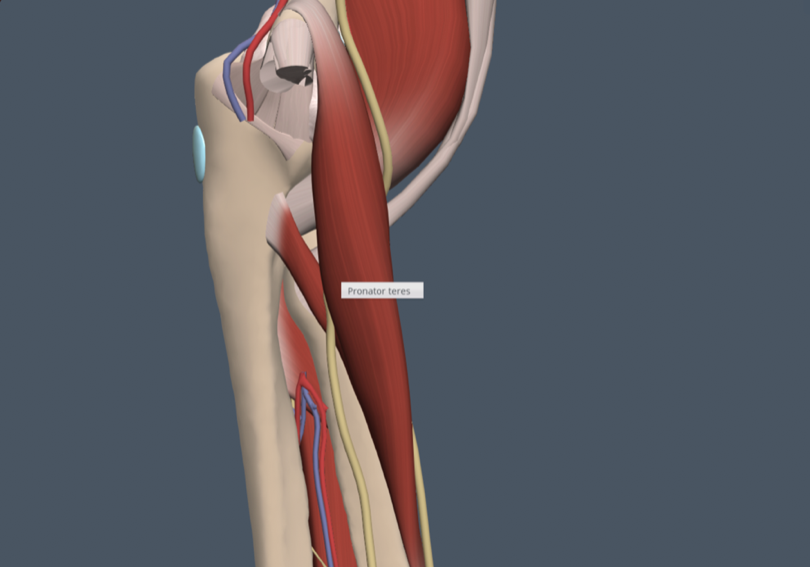
Common Median Nerve Injuries
Common Median Nerve Injuries By: Madison Mott Did you know!? Aside from the most common upper extremity nerve compression, carpal tunnel syndrome (CTS), there are several additional median nerve injuries. Pronator SyndromeCompression of the median nerve between the two heads of pronator teres. Result of recurrent, forceful gripping, forearm rotation, or elbow flexion. Signs include…
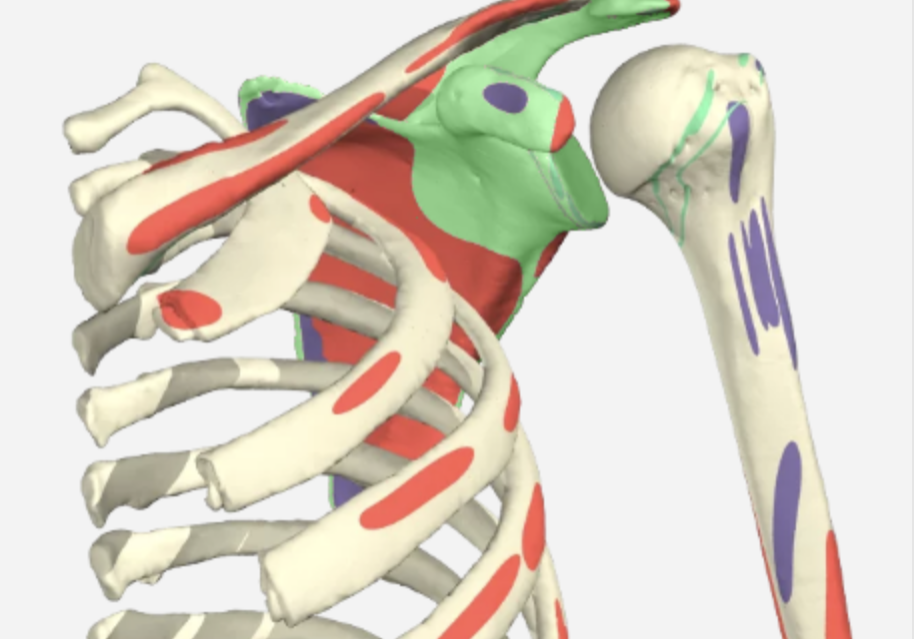
Read MoreThe function of the Glenohumeral Joint Ligaments
Glenohumeral Joint Ligaments The Glenohumeral (GH) joint is composed of the head of the humerus and the glenoid fossa. The fossa is relatively small compared to the humeral head, making the joint highly mobile, which also leads to an increased risk of instability. The glenoid labrum is a fibrocartilagenous rim attached around the…
Read MoreOutcomes of Rigid Night Splinting and Activity Modification in the Treatment of Cubital Tunnel Syndrome
Shah, C. M., Calfee, R. P., Gelberman, R. H., & Goldfarb, C. A. (2013). Outcomes of rigid night splinting and activity modification in the treatment of cubital tunnel syndrome (night splint for cubital tunnel syndrome). The Journal of Hand Surgery, 38(6), 1125–1130.e1. https://doi.org/10.1016/j.jhsa.2013.02.039 By: Sophia Grimm The Skinny: The purpose of this study was to…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.




Thank you very much! I always thought, how can I tell to my patients all this information very short and understandable! Thank you for your tips!!
Great Post! These tips and providing comprehensive support and guidance, healthcare professionals can help patients effectively manage hand osteoarthritis and improve their overall quality of life. Collaboration between patients and healthcare providers is essential to developing personalized treatment plans that address the unique needs and goals of each individual.