Which is better: Splinting the MCP or PIP joint when managing Trigger Finger?
Filed under Orthoses, Treatments
Teo, S. H., Ng D. C., Wong, Y.K.(2018). Effectiveness of proximal interphalangeal joint blocking orthosis vs metacarpophalangeal joint blocking orthosis in trigger digit: A randomized clinical trial. Journal of Hand Therapy, 1-7.
The Skinny- This study compared PIP joint immobilization via an Oval-8TM with a custom MCP blocking trigger finger orthosis treatment.

In the Weeds – Patient (n=35) with Trigger Finger (n=43) were analyzed. Twenty-three patients were allocated to the PIP joint splinting group and 20 patients were in the MCP splinting group. Patients wore the orthosis for eight weeks – these were MCP splint for trigger finger, MCP blocking splint and pip joint splint.
Pain reduction was observed in both groups, but pain reduction was greater with PIP joint splinting compared to the MCP joint splinting group. There was only significant improvement in QuickDASH for the PIP splinting Group. Patients wore the pip joint splint significantly longer during the day compared to the MCP splinting group, most likely due to improved comfort.
Bringing it Home- Findings suggests both orthoses are effective in reducing QuickDASH scores, reducing pain and improving overall trigger finger symptoms based on Green’s Classification. However, the pip joint immobilization splint was better for improved function and improved compliance.
Rationale for rating. Small sample size. All patients with comorbidities were excluded limiting the generalizability of finding. Immobilizing the PIP joint compared to the MCP allows more function and improved compliance. When immobilizing the MCP you limit intrinsic grasp which is a necessity for function. The authors recommend wearing the orthosis for a 4 week duration for 24 hours in order to reduce triggering symptoms followed by night-time splint wear for another 3-4 weeks.
10 Comments
Leave a Comment
More To Read
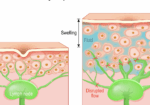
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy
Comparing Edema and Lymphedema: Understanding the Differences and Treatment Approaches in Hand Therapy As hand therapists we often encounter patients presenting with swollen arms, hands, and/ or fingers, often attributing these symptoms to various conditions. Two commonly confused terms in this area are “edema” and “lymphedema.” While both involve swelling, they have distinct causes, presentations,…
Functional Home Exercises for Patients with Wrist Instability
Functional Home Exercises for Patients with Wrist Instability Ever wondered what brushing your teeth, dressing, making a U-turn, and playing sports have in common? They all rely on a stable wrist. Wrist stability is crucial for everyday activities, supporting wrist proprioception, coordination, motor control, stability, and mobility (Wietlisbach, 2019). For patients recovering from a wrist…
Factors that influence orthosis adherence in patients with acute traumatic tendon injuries to the hand
Savaş, S., & Aydoğan, Ç. (2020). Factors affecting orthosis adherence after acute traumatic hand tendon repairs: A prospective cohort study. Journal of Hand Therapy, S0894113020301848. https://doi.org/10.1016/j.jht.2020.10.005 World Health Organization. (2003). Adherence to long-term therapies: evidence for action. World Health Organization. The Skinny Adherence to orthosis wear is vital for protecting healing tendons after a traumatic tendon…
Pain management techniques for Wrist Fractures
Pain management techniques for wrist fractures Distal radius fractures account for 17.5% of all fractures with a median age of 60.23(Candela et.al, 2022). Pain management is a significant part of post wrist fracturetreatment due to limitations that pain incurs. Chronic Regional Pain Syndrome (CRPS) canoccur along with a distal radius fracture but will not be…
Sign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.






This is great! Keep them coming!
really interesting- thanks
We’re glad you liked it. We will keep them coming.
Love this!!! Thank you.
Glad you liked it!
Thanks for sharing !
What about PIP range of motion ?
Typically we instruct the patient with prom and to avoid active if it is causing the triggering to occur.
Thanks for sharing!
Important to know.
This is great – curious if there was a time frame of symptoms present for inclusion criteria and or for splinting to be effective? ie if the patient had triggering for less than 3 months splinting was found to be effective; or were patients who had symptoms for longer than x-amount of weeks/months were not included, etc etc? I have always been under the impression if symptoms are too severe/present for more than 4 weeks cortisone injection is kind of the gold standard as splinting is less effective at that point? Thank you!
Yes, the longer the condition goes on the more difficult it is to treat. From personal experience, I have had patients resolve their symptoms for trigger fingers that have been going on for 6 months