By: Megan Prather
The prevalence of external fixation with pins in the upper extremity setting and the high rates of pin site infection make identifying a protocol for pin site care important for therapists. Across literature, there are many different pin site care protocols varying in frequency, solutions, materials, and manual cleaning. Despite many studies and reviews, there is no overall consensus or gold standard for pin site care after fixation (Kazmers, Fragomen, & Rozbruch, 2016). Because of the types of tissue present around certain pin sites in the upper extremity, some sites are prone to infection regardless of the site care that is done (Altman, 2011).
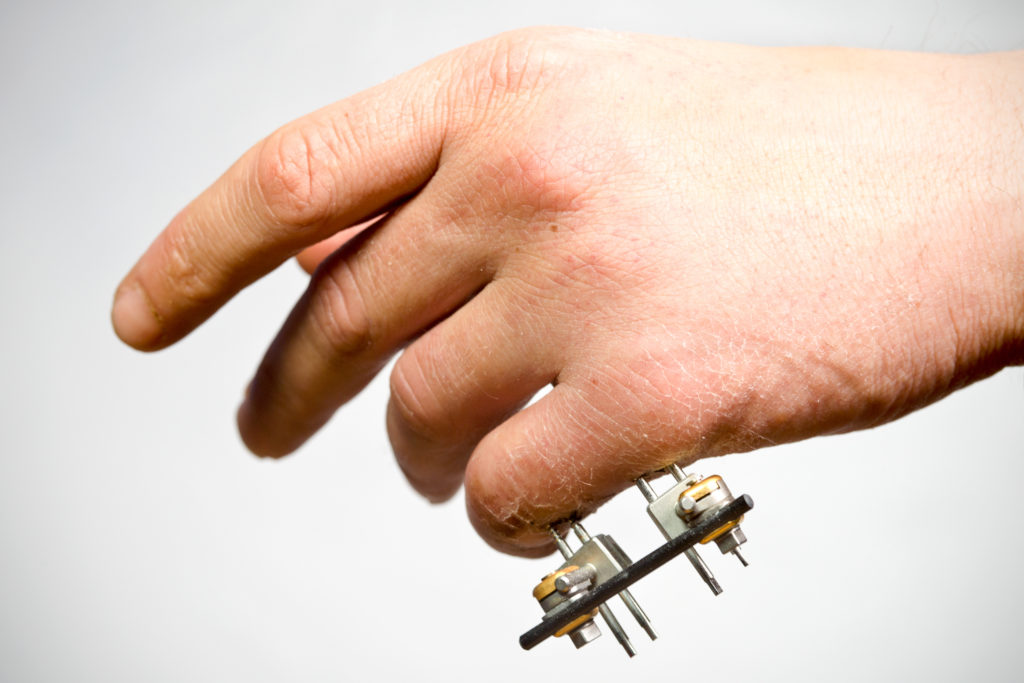
This post outlines several protocols and points from the literature, but it is important to keep in mind that pin site care is dependent on each surgeon’s techniques and preferences. It is also important to note that pin site care instruction includes not only educating the patient on step-by-step instruction for cleaning the sites, but also includes strategies for pain management and recognition of the signs and symptoms of infection.
Showers
Especially in children, a pin site care protocol of daily showers starting 5 days after surgery shows to be just as effective as other more complicated routines (Gordon, Kelly-Hahn, Carpenter, & Schoenecker, 2000). Later studies also found daily showers to be effective after the first 15 days of site care with sterile gauze and iodine (Cavusoglu et al., 2009). Regardless of pin site care approach, typical daily showering can be and often is used as a helpful adjunct to the protocol given to patients.
- Instruct patients in daily showering, letting water run over pin sites
- Use a soft toothbrush and antibacterial soap to gently clean the area around the pin
Sterile Gauze
A common method of pin site care includes using sterile gauze, soaked in various solutions, to clean the pin and the area around it. Sterile dressings are also used after various methods of cleaning in a compressive manner to dress the pin sites until the next cleaning (Altman, 2011). Studies have looked at the use of many different solutions on sterile gauze- including Povidone iodine (10%), sodium hypochlorite (0.05%), 1:1 hydrogen peroxide and saline solution, and plain saline- finding a wide range of infection rates and making a recommendation for the best solution difficult (Cavusoglu et al., 2009; Bisaccia et al., 2016; Kazmers, Fragomen, & Rozbruch, 2016; Altman, 2011). One study in 2016 suggested that a sodium hypochlorite (0.05%) solution results in lower infection rates than Povidone iodine (10%) (Bisaccia et al., 2016).
- Instruct your patient to dampen sterile gauze with Povidone iodine (10%), sodium hypochlorite (0.05%), 1:1 hydrogen peroxide and saline solution, or simply saline.
- Identify if the surgeon has a preferred solution for pin care
- Use the damp sterile gauze to clean the area around the base of the pin, clearing away crusts, and wipe up and away from the skin along the pin on all sides
- Apply dry sterile gauze compressively around the pin sites to dress after cleaning
Cotton-Tipped Applicator
While evidence for the best cleaning solution remains absent, the use of cotton-tipped applicators in the cleaning of pin sites is well documented (Kazmers et al., 2016).
- Instruct your patient to use a cotton-tipped applicator soaked with a 1:1 hydrogen peroxide and saline solution (or Povidone iodine (10%), sodium hypochlorite (0.05%), or saline)
- Clean around the base of the pin site and wipe up and away from the skin along the pin on all sides
- Wrap in dry sterile gauze after cleaning
Kurgan Method
Some research has indicated that the Kurgan method of pin site care has a lower incidence of infection than other approaches (Ktiistakis, Guerado, & Giannoudis, 2015). This method is also known as the Russian style of pin site care and is meant to be used after pin sites have started to heal (Adams, 2019).
- Instruct your patient to use gauze dampened with Pink Hydrex (let the gauze sit for a few minutes to allow the alcohol to evaporate- this may be more comfortable for the patient)
- Clean from the entry site wiping up and away from the skin along the pin (do not wipe towards the skin)
- Leave any adherent crusts alone unless infected
- Dress with sterile gauze dampened with Pink Hydrex (unless infected or raw incisions are present)
- Repeat weekly
Nothing
Despite the numerous tools and solutions available for pin cleaning, some surgeons and research studies suggest simply leaving the pin sites alone. Allowing the body to manage its own health and cleanliness may be just as effective as providing help. Some researchers also discuss the tissue trauma that can be caused by traditional pin care techniques such as moving the skin around the pin with a swab, scraping away scabs and dried exudate, and using solutions like hydrogen peroxide which can also harm good cells in the area. These practices may cause tissue damage and death which impact the body’s immune response in dealing with the trauma (Gordon, Kelly-Hahn, Carpenter, & Schoenecker, 2000).
- Instruct your patient to be aware and careful of their pin cites (trying to avoid getting them dirty), but not to do any special cleaning of the skin around the pins.
How Often?
Clinical practice and studies suggest that either daily or weekly care is appropriate and equally effective in reducing infection (Lethaby, Temple, & Santy, 2011). Talk with the surgeon and consider relevant patient factors in determining the frequency with which pin care should take place for each individual patient.

No One Right Answer
All of the pin site care strategies mentioned above can be effective in curbing infection after surgery until the pins can be removed (pin site care after removal). Whichever method is chosen for cleaning wipe up and away from the pin site with the cleaning agent, not towards it. Infection is very common at pin sites and any method of pin site care may still result in some degree of infection. It is important to educate patients on the signs and symptoms of infection and to alert the physician or surgeon if infection is detected as antibiotics may be needed. When choosing a method for pin site care consider the most supported methods by research, patient factors that influence following the steps required for each method, and surgeon preference to determine the best method for you and your patients.
References
Adams, L. (2019). Pin site care (Reference No. TC7(04)). Retrieved from Salford Royal NHS Foundation Trust website: https://www.srft.nhs.uk/EasysiteWeb/getresource.axd?AssetID=33132&type=full&servicetype=Inline#:~:text=The%20Kurgan%20rationale%3A%20reduces%20pin,and%20dress%20the%20pin%20sites.
Altman, E. (2011). Therapist’s management of the stiff elbow. In T.M. Skirven, A.L. Osterman, J.M. Fedorczyck & P.C. Amadio (Eds.), Rehabilitation of the Hand and Upper Extremity (6th ed., pp. 1075-1088). Mosby.
Bisaccia, M., Manni, M., Colleluori, G., Falzarano, G., Medici, A., Meccariello, L., … Caraffa, A. (2016). The management of pin-carae in external fixation technique: Povidone-iodine versus sodium hypochlorite 0.05% (Amukina-med®) medications. Euromediterranean Biomedical Journal, 11, 81-87.
Cavusoglu, A.Tu., Er, M.S., Inal, S.., Ozsoy, M.H., Dincel, V.E., & Sakaogullari, A. (2009). Pin site care during circular external fixation using two different protocols. Journal of Orthopaedic Trauma, 23(10), 724-730. doi: 10.1097/BOT.0b013e3181abbc31
Gordon, J.E., Kelly-Hahn, J., Carpenter, C.J., & Schoenecker, P.L. (2000). Pin site care during external fixation in children: Results of a nihilistic approach. Journal of Pediatric Orthopaedics, 20(2), 163-165
Kazmers, N. H., Fragomen, A. T., & Rozbruch, S. R. (2016). Prevention of pin site infection in external fixation: a review of the literature. Strategies in trauma and limb reconstruction, 11(2), 75–85. https://doi.org/10.1007/s11751-016-0256-4
Ktiistakis, I., Guerado, E., & Giannoudis, P.V. (2015). Pin-site care: Can we reduce the incidence of infections?. Injury, 46(3), S35-S39. https://doi.org/10.1016/S0020-1383(15)30009-7
Lethaby, A., Temple, J., & Santy, J. (2011). Pin site care for preventing infections associated with external bone fixators and pins. [PDF]. Retrieved from https://pdfs.semanticscholar.org/a682/5a9c497933af615fa718bb6ebfcec0a621fc.pdf
More To Read
Title: Understanding De Quervain’s Pathology: A Comprehensive Exploration of Special Tests
Understanding De Quervain’s Pathology: A Comprehensive Exploration of Special Tests By: Miranda Materi De Quervain’s and Special Tests De Quervain’s tenosynovitis is a condition characterized by inflammation of the tendons on the thumb side of the wrist, causing pain and discomfort. These tendons include Abductor Pollicis Longus (APL) and Extensor Pollicis Brevis as they pass through…
Read MoreCarpal Tunnel Syndrome: How does traditional hand therapy compare with neurodynamic therapy?
Hamzeh, H., Mohammad, M., Alghwiri, A., & Hawamdeh, Z. (2021). The long-term effect of neurodynamics vs. exercise therapy on pain and function in people with carpal tunnel syndrome: A randomized parallel-group clinical trial. Journal of Hand Therapy, 34, 521-530. The Skinny: Carpal tunnel is the most common peripheral nerve compression problem. There is now some…
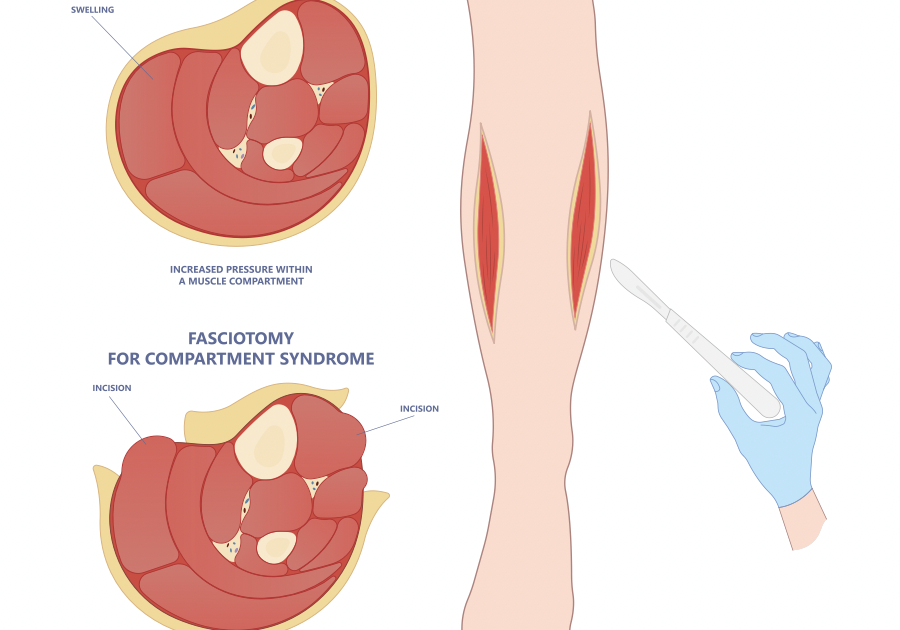
Read MoreExertional (Chronic) Compartment Syndrome of The Hand
By: Tommi Long What is it? Chronic exertional compartment syndrome (CECS) is an exercise-induced condition affecting the muscles and nerves, leading to pain, swelling, and reduced muscle function due to increased pressure and restricted circulation. While most commonly, it impacts the arms and legs, it is rare to happen in the hand(s). CECS is most…
Read MoreSign-up to Get Updates Straight to Your Inbox!
Sign up with us and we will send you regular blog posts on everything hand therapy, notices every time we upload new videos and tutorials, along with handout, protocols, and other useful information.